Understanding ACA Claims Denials and Why They Matter
The Affordable Care Act (ACA) plays a pivotal role in health insurance access, yet many enrollees face challenges stemming from claims denials. In 2023, nearly 20% of all health claims in the federally facilitated Marketplace (HealthCare.gov) were denied, with a staggering 37% denial rate for out-of-network claims. This statistic highlights the considerable hurdles insured individuals encounter when seeking medical care.
In-Network vs. Out-of-Network: The Denial Rates Broken Down
In-Network Claims – The denial rate for in-network services fluctuated significantly across different insurers and states, ranging from as low as 1% to a troubling 54%. This inconsistency suggests that enrollees in some regions may have drastically different experiences based on where they live or which insurance provider they choose. Out-of-Network Claims – With an overall denial rate of 37%, these figures underscore the importance of understanding your network options to minimize out-of-pocket expenses and potential denials.
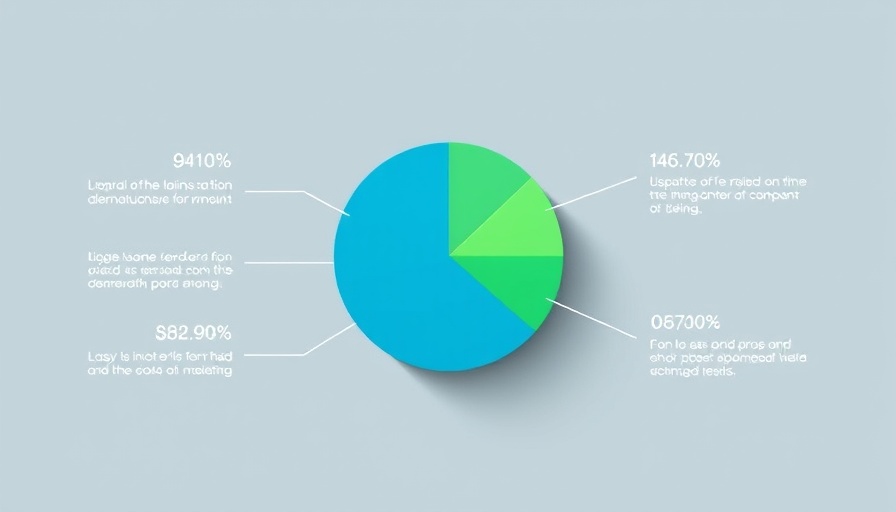
Why Do Insurers Deny Claims?
Among those claims that were denied, many entrants were turned away for reasons that are not clearly defined. It is concerning that 34% of these denials fell into an “Other” category, closely followed by administrative issues (18%). The lack of transparency regarding the reasons behind denials demonstrates the need for clearer communication from insurers. Only 6% of claims were denied due to a lack of medical necessity, which raises questions about the criteria used in the decision-making process.
The Appeals Process: An Uphill Battle
Consumers rarely appeal denied claims, facing a daunting reality where less than 1% file appeals against their insurers' decisions. Even when appeals are made, the majority are unsuccessful, as insurers uphold about 56% of their initial decisions. This trend raises concerns about the effectiveness of the current appeal system and whether enrolled individuals fully understand their rights and options regarding these processes.
Consumer Experience and the Road Ahead
Reports indicate that 58% of insured adults encountered issues with their health insurance, with denied claims contributing to financial strain for many, particularly among those struggling with medical bills. As consumers navigate this complicated landscape, understanding the implications of claims denials and the appeals process remains crucial. Awareness of their rights can empower consumers to take informed steps in safeguarding their healthcare access.
 Add Row
Add Row  Add
Add 




Write A Comment